Summary
Written by Dr. Muhammad Babar Bilal, PharmD, MPhil (Pharmaceutical Chemistry), BS Clinical Psychology. Dr. Bilal specializes in diabetes care, supplement safety, and patient counseling.
Personalised Nutrition Plans for Diabetes Management
Managing diabetes effectively requires a thoughtful approach to nutrition, tailored to individual health needs, preferences, and lifestyles.
A personalised nutrition plan can empower individuals with diabetes to make informed dietary choices, leading to better blood sugar control, improved overall health, and enhanced quality of life.
Below are comprehensive guidelines to create an effective personalised nutrition plan for diabetes management.
Understanding the Basics of Nutrition in Diabetes
Carbohydrate Counting: Carbohydrates have the most significant impact on blood sugar levels.
Understanding how to count carbs allows for better management of insulin doses and overall glycaemic control.
Incorporate complex carbohydrates like whole grains, legumes, and vegetables, while being mindful of portion sizes.
Glycaemic Index (GI): Foods with a low GI are digested more slowly, leading to a gradual increase in blood sugar levels.
Prioritize low to moderate GI foods such as whole grains, fruits, and non-starchy vegetables.
Balanced Meals: Ensure each meal contains a balance of carbohydrates, proteins, and healthy fats.
Proteins help in muscle maintenance and satiety, while healthy fats (like those from avocados, nuts, and olive oil) support heart health.
Personalised Nutrition Guidelines 1. Assess Individual Needs
Medical History: Consult healthcare professionals to understand specific health issues, allergies, or dietary restrictions.
Activity Levels: Tailor the nutritional plan according to daily activity levels, as active individuals may require more energy (calories) and nutrients.
Cultural Preferences: Incorporate foods and cooking methods that resonate with personal and cultural preferences, fostering adherence to the plan.
2. Set Realistic Goals
Short-term and Long-term Goals: Set achievable goals, such as reducing blood sugar levels, losing weight, or enhancing nutrient intake.
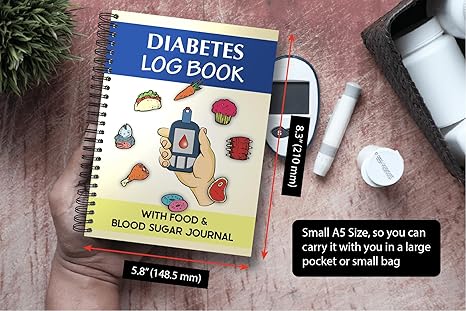
Monitor Progress: Use tools like food diaries, nutrition apps, or regular consultations with dietitians to track advancements towards goals.
3. Meal Planning and Preparation
Create Weekly Menus: Design weekly menus that include a variety of low-glycaemic foods. This helps eliminate impulsive eating decisions.
Portion Control: Use measuring tools or portion templates to ensure appropriate serving sizes, minimising the risk of overeating.
Meal Prep: Cooking in batches and preparing meals ahead of time can facilitate healthy eating during busy times.
4. Education on Food Choices
Read Nutrition Labels: Learn how to read labels to make informed choices, especially regarding carbohydrates, sugars, and serving sizes.
Healthy Swaps: Identify unhealthy ingredients and find healthier alternatives. For instance, use whole grain bread instead of white bread, or swap sugary snacks for fresh fruits or nuts.
5. Hydration
Stay Hydrated: Encourage water consumption as the primary beverage. Limit sugary drinks and juices, as they can spike blood glucose levels.
6. Collaboration with Professionals
Engage a Registered Dietitian: Collaborate with a registered dietitian specialised in diabetes care for personalised advice, ongoing support, and adjustments to the plan as needed.
Interdisciplinary Approach: Involve a multidisciplinary team, including doctors, nutritionists, and diabetes educators, to ensure comprehensive care.
Conclusion
A personalised nutrition plan for diabetes management is not just about restrictions; it’s about empowering individuals to indulge in a variety of wholesome foods while managing their blood sugar levels effectively.
By tailoring nutrition to individual needs, preferences, and health goals, diabetics can make sustainable lifestyle changes that result in improved health outcomes and well-being.
Always remember to regularly review and adapt the plan to meet changing health needs and advancements in diabetes management strategies.